Live on the homepage now!
Reader Supported News
The ethics issues are dizzying. The guy was once Leader of the Free World and intends to resume the position, which is his by right. As such, he deals in foreign policy in behalf of the people of the United States. Their interests are not identical to those of oil trillionaires. Clearly, the gentleman is steering us into uncharted waters, as he has so assiduously done for many years. He occupies a realm previously belonging to fiction.
I was worried when the submersible went down with the Titanic that he might’ve paid a quarter-million to go down and view the wreckage and see how he could bring it up and monetize it piece by piece, but luckily he did not. He is busy steering the Republican Party toward the iceberg of established law and if he hits it and it splits into chunks and he sells them to the Saudis to chill their drinks, then there is no point in teaching law anymore. Look back in history: did Trump University have a law school? No, it did not.
If the law doesn’t apply to the big guys, then the peons and pissants are not going to abide by it either. Gangs will roam the streets, taking what they will, and we whose parents brought us up not to lie or steal will need to find hired guns to keep the mob at bay. It’ll be the Wild West but on steroids.
My fellow Democrats were wrong when we scorned Lawn Order as inherently repressive back when Republicans were in favor of it. Lawn Order is to the benefit of the children, the most vulnerable among us, and the elderly and infirm, and dreamy idealists such as my fellow English majors. I see them in the park with their little notebooks, writing something about trees and clouds. These people are a sitting target for any bully with a paring knife. This is why defunding the police is the biggest fraud to come down the pike since the sale of the Brooklyn Bridge. We who sit in the park and write sonnets need crooks to be afraid of cops. Criminals tend to be incredibly stupid but they know that guns shoot and bullets hurt.
You and I do not have the skill set that the Trump family has. Think what you will about Hunter Biden, he didn’t have the savvy of Jared Kushner who got the Saudis to drop two billion into his investment firm Affinity. What Taylor Swift is to teenage girls, Donald is to grown-up vandals. But we need the Trumps to know there are Jack Smiths on the job. And call me naïve but when I tune in the ball game, I honestly believe the home plate ump is not on the other team’s payroll. I can’t prove it but this faith makes it possible to enjoy the game, and if there’s no pleasure in it then why are we paying so much attention?
READ MORE  People rally to show support for the Biden administration's student debt relief plan in front of the Supreme Court on Feb. 28, in Washington, D.C. (photo: Kent Nishimura/Los Angeles Times)
People rally to show support for the Biden administration's student debt relief plan in front of the Supreme Court on Feb. 28, in Washington, D.C. (photo: Kent Nishimura/Los Angeles Times)
The court's six conservatives invalidated President Biden's plan to wipe away $400 billion in student debt
The court invalidated Biden’s program — re-saddling millions with thousands of dollars in debt they didn’t have yesterday — with a 6-3 vote, along ideological lines. Justice Elena Kagan wrote the dissenting opinion. “The result here is that the Court substitutes itself for Congress and the Executive Branch in making national policy about student-loan forgiveness,” she wrote. “Congress authorized the forgiveness plan (among many other actions); the Secretary put it in place; and the President would have been accountable for its success or failure. But this Court today decides that some 40 million Americans will not receive the benefits the plan provides, because (so says the Court) that assistance is too “significant.'”
The White House announced after the decision came down that Biden “will make clear he’s not done fighting yet” and will announce “new actions to protect student loan borrowers.”
Biden announced the plan — which would have primarily impacted low-income Americans saddled with student debt — last August. Republicans threw a fit, describing the plan as “socialism,” “unfair,” and a “slap in the face” to those who paid for college. “I will never apologize for helping Americans, especially not to the same folks who voted for a $2 trillion tax cut that mainly benefited the wealthiest Americans and the biggest corporations,” Biden responded.
The conservative outrage over the government trying to make things easier for tens of millions Americans soon begat a lawsuit alleging Biden couldn’t forgive student debt with Congress signing off on it first. The 8th Circuit Court of Appeals put a temporary hold on the plan last October. The Supreme Court struck the death blow on Friday.
Even after adjusting for inflation, average college tuition has risen by 169 percent in the last 40 years, according to data from the Georgetown University Center on Education and the Workforce, and 70 percent of American students now graduate with some amount of debt.
The ruling came on the final day of the court’s nine-month term, and a day after it struck down race-based affirmative action in college admissions. The court ruled that businesses can discriminate against gay people earlier on Friday.
READ MORE  Senior NATO officials told VICE News that General Sergei Surovikin was believed to be held in Rostov-on-Don, a city seized in the failed mutiny. (photo: Russian Defense Ministry)
Senior NATO officials told VICE News that General Sergei Surovikin was believed to be held in Rostov-on-Don, a city seized in the failed mutiny. (photo: Russian Defense Ministry)
Senior NATO officials told VICE News that General Sergei Surovikin was believed to be held in Rostov-on-Don, a city seized in the failed mutiny.
General Sergei Surovikin, nicknamed “General Armageddon” for commanding Russian air forces in Syria, has been detained in southern Russia, the NATO officials said. They added he was probably in the military headquarters in Rostov-on-Don, the epicentre of Wagner’s short lived coup, for questioning about his relationship with Wagner warlord Yevgeny Prigozhin, who has been forced into exile in Belarus by Putin.
“He was last seen in Rostov and while possible, I haven’t seen any reason to think he has been moved,” a NATO official told VICE News.
The detention of Surovikin was first reported by the UK’s Financial Times newspaper and confirmed by two NATO officials on the condition of anonymity. Surovikin has not been seen in public since Saturday’s failed putsch aimed at Russian military leaders that Prigozhin said were betraying the Ukraine war effort.
His daughter, Veronika, denied that he had been detained when contacted by Baza, a Russian media outlet with ties to the security services. “Nothing happened to him, he is at his workplace as usual,” she said.
While Wagner and Russian military officials have had bombastically tense relations over Ukraine, Surovikin is considered close to Prigozhin and said to be an honorary Wagner member. The New York Times has previously reported that US officials believe Surovikin had prior knowledge of Prigozhin’s plan.
“It’s hard to say if it's a formal charge or just a ‘frank discussion of the weekend’s events,’ but clearly Putin suspects Surovikin of at least not reporting coup-like discussions,” said one official. “Prigozhin and Surovikin have been allies against the defence establishment in the past, certainly in Syria.”
Last week, Prigozhin announced his intent to arrest key ministry of defence and Russian army figures for improperly managing the war effort in Ukraine. By Saturday morning, his mercenary troops had occupied Rostov without resistance and drove within 120 miles of Moscow – shooting down multiple Russian Army helicopters and a plane along the way – before both sides agreed to stand down in a deal brokered by Belarusian President and Kremlin ally Alexander Lukashenko.
The senior NATO official said if Putin is forced to purge Surovikin, it could be a greater loss than the tens of thousands of well trained and equipped Wagner troops whose future fighting for post-coup Russia remains very much in doubt.
“It’s unclear what the plan for Wagner is,” said the official. “There’s been reports of some heavy weapons handovers and Belarus is clearly building facilities but there’s not much actual movement in any direction. But the involvement or loss of Surovikin might sting as he’s a complete bastard but basically competent. He designed the defensive lines that Ukraine is currently trying to crack.”
The second official refused to speculate on how far Putin would go in any loyalty purge but said the regime’s current restraint could be a sign of insecurity.
“If Putin knew who to purge, he’d purge them,” said the second official, who added that the appearance of indecision by Putin might be shaking the elite’s confidence in him.
“It’s the uncanny silence from the Russian elites that has all of us, probably including Putin spooked,” said the second official. “Key military and economic figures, the elites that Putin relies on as much as they rely on them, haven’t been as vocally loyal as we, or Putin, would expect.”
READ MORE  Karen Pollitz, a senior fellow at KFF, has written repeatedly about the lack of data on how often insurance companies deny claims. (photo: Alyssa Schukar/ProPublica)
Karen Pollitz, a senior fellow at KFF, has written repeatedly about the lack of data on how often insurance companies deny claims. (photo: Alyssa Schukar/ProPublica)
Insurers’ denial rates — a critical measure of how reliably they pay for customers’ care — remain mostly secret to the public. Federal and state regulators have done little to change that.
After all, an insurance company that routinely rejects recommended care could damage both your health and your finances. The question becomes ever more pressing as many working Americans see their premiums rise as their benefits shrink.
Yet, how often insurance companies say no is a closely held secret. There’s nowhere that a consumer or an employer can go to look up all insurers’ denial rates — let alone whether a particular company is likely to decline to pay for procedures or drugs that its plans appear to cover.
The lack of transparency is especially galling because state and federal regulators have the power to fix it, but haven’t.
ProPublica, in collaboration with The Capitol Forum, has been examining the hidden world of insurance denials. A previous story detailed how one of the nation’s largest insurers flagged expensive claims for special scrutiny; a second story showed how a different top insurer used a computer program to bulk-deny claims for some common procedures with little or no review.
The findings revealed how little consumers know about the way their claims are reviewed — and denied — by the insurers they pay to cover their medical costs.
When ProPublica set out to find information on insurers’ denial rates, we hit a confounding series of roadblocks.
In 2010, federal regulators were granted expansive authority through the Affordable Care Act to require that insurers provide information on their denials. This data could have meant a sea change in transparency for consumers. But more than a decade later, the federal government has collected only a fraction of what it’s entitled to. And what information it has released, experts say, is so crude, inconsistent and confusing that it’s essentially meaningless.
The national group for state insurance commissioners gathers a more detailed, reliable trove of information. Yet, even though commissioners’ primary duty is to protect consumers, they withhold nearly all of these details from the public. ProPublica requested the data from every state’s insurance department, but none provided it.
Two states collect their own information on denials and make it public, but their data covers only a tiny subset of health plans serving a small number of people.
The minuscule amount of details available about denials robs consumers of a vital tool for comparing health plans.
“This is life and death for people: If your insurance won’t cover the care you need, you could die,” said Karen Pollitz, a senior fellow at KFF (formerly known as the Kaiser Family Foundation) who has written repeatedly about the issue. “It’s all knowable. It’s known to the insurers, but it is not known to us.”
The main trade groups for health insurance companies, AHIP (formerly known as America’s Health Insurance Plans) and the Blue Cross Blue Shield Association, say the industry supports transparency and complies with government disclosure requirements. Yet the groups have often argued against expanding this reporting, saying the burdens it would impose on insurance companies would outweigh the benefits for consumers.
“Denial rates are not directly comparable from one health plan to another and could lead consumers to make inaccurate conclusions on the robustness of the health plan,” Kelly Parsons, director of media relations for the Blue Cross Blue Shield Association, said in an email.
The trade groups stress that a substantial majority of patient claims are approved and that there can be good reasons — including errors and incomplete information from doctors — for some to be denied.
“More abstract data about percentages of claims that are approved or denied have no context and are not a reliable indicator of quality — it doesn’t address why a claim was or was not approved, what happened after the claim was not approved the first time, or how a patient or their doctor can help ensure a claim will be approved,” AHIP spokesperson Kristine Grow said in a written response to questions from ProPublica. “Americans deserve information and data that has relevance to their own personal health and circumstances.”
The limited government data available suggests that, overall, insurers deny between 10% and 20% of the claims they receive. Aggregate numbers, however, shed no light on how denial rates may vary from plan to plan or across types of medical services.
Some advocates say insurers have a good reason to dodge transparency. Refusing payment for medical care and drugs has become a staple of their business model, in part because they know customers appeal less than 1% of denials, said Wendell Potter, who oversaw Cigna’s communications team for more than a decade before leaving the industry in 2008 to become a consumer advocate.
“That’s money left on the table that the insurers keep,” he said.
At least one insurer disputes this. Potter’s former employer, Cigna, said in an email that his “unsubstantiated opinions” don’t reflect the company’s business model. In a separate written statement, Cigna said it passes on the money it saves “by lowering the cost of health care services and reducing wasteful spending” to the employers who hire it to administer their plans or insure their workers.
The few morsels insurers have served up on denials stand in stark contrast to the avalanche of information they’ve divulged in recent years on other fronts, often in response to government mandates. Starting last year, for example, insurers began disclosing the prices they’ve negotiated to pay medical providers for most services.
Experts say it’ll take similar mandates to make insurers cough up information on denials, in part because they fear plans with low denial rates would be a magnet for people who are already ailing.
“Health plans would never do that voluntarily, would give you what their claim denial rates are, because they don’t want to attract sicker people,” said Mila Kofman, who leads the District of Columbia’s Affordable Care Act exchange and previously served as Maine’s superintendent of insurance.
About 85% of people with insurance who responded to a recent KFF survey said they want regulators to compel insurers to disclose how often they deny claims. Pollitz, who co-authored a report on the survey, is a cancer survivor who vividly recalls her own experiences with insurance denials.
“Sometimes it would just make me cry when insurance would deny a claim,” she said. “It was like, ‘I can’t deal with this now, I’m throwing up, I just can’t deal with this.’”
She should have been able to learn how her plan handled claims for cancer treatment compared with other insurers, she said.
“There could be much more accountability.”
In September 2009, amid a roiling national debate over health care, the California Nurses Association made a startling announcement: Three of the state’s six largest health insurers had each denied 30% or more of the claims submitted to them in the first half of the year.
California insurers instantly said the figures were misleading, inflated by claims submitted in error or for patients ineligible for coverage.
But beyond the unexpectedly high numbers, the real surprise was that the nurses association was able to figure out the plans’ denial rates at all, by using information researchers found on the California Department of Managed Health Care’s website.
At the time, no other state or federal regulatory agency was collecting or publishing details about how often private insurers denied claims, a 2009 report by the Center for American Progress found.
The Affordable Care Act, passed the following year, was a game changer when it came to policing insurers and pushing them to be more transparent.
The law took aim at insurers’ practice of excluding people with preexisting conditions, the most flagrant type of denial, and required companies offering plans on the marketplaces created under the law to disclose their prices and detail their benefits.
A less-noticed section of the law demanded transparency from a much broader group of insurers about how many claims they turned down, and it put the Department of Health and Human Services in charge of making this information public. The disclosure requirements applied not only to health plans sold on the new marketplaces but also to the employer plans that cover most Americans.
The law’s proponents in the Obama administration said they envisioned a flow of accurate, timely information that would empower consumers and help regulators spot problematic insurers or practices.
That’s not what happened.
The federal government didn’t start publishing data until 2017 and thus far has only demanded numbers for plans on the federal marketplace known as Healthcare.gov. About 12 million people get coverage from such plans — less than 10% of those with private insurance. Federal regulators say they eventually intend to compel health plans outside the Obamacare exchanges to release details about denials, but so far have made no move to do so.
Within the limited universe of Healthcare.gov, KFF’s analyses show that insurers, on average, deny almost 1 in 5 claims and that each year some reject more than 1 in 3.
But there are red flags that suggest insurers may not be reporting their figures consistently. Companies’ denial rates vary more than would be expected, ranging from as low as 2% to as high as almost 50%. Plans’ denial rates often fluctuate dramatically from year to year. A gold-level plan from Oscar Insurance Company of Florida rejected 66% of payment requests in 2020, then turned down just 7% in 2021. That insurer’s parent company, Oscar Health, was co-founded by Joshua Kushner, the younger brother of former President Donald Trump’s son-in-law Jared Kushner.
An Oscar Health spokesperson said in an email that the 2020 results weren’t a fair reflection of the company’s business “for a variety of reasons,” but wouldn’t say why. “We closely monitor our overall denial rates and they have remained comfortably below 20% over the last few years, including the 2020-2021 time period,” the spokesperson wrote.
Experts say they can’t tell if insurers with higher denial rates are counting differently or are genuinely more likely to leave customers without care or stuck with big bills.
“It’s not standardized, it’s not audited, it’s not really meaningful,” Peter Lee, the founding executive director of California’s state marketplace, said of the federal government’s information. Data, he added, “should be actionable. This is not by any means right now.”
Officials at the Centers for Medicare … Medicaid Services, which collects the denial numbers for the federal government, say they’re doing more to validate them and improve their quality. It’s notable, though, that the agency doesn’t use this data to scrutinize or take action against outliers.
“They’re not using it for anything,” Pollitz said.
Pollitz has co-authored four reports that call out the data’s shortcomings. An upshot of all of them: Much of what consumers would most want to know is missing.
The federal government provides numbers on insurers’ denials of claims for services from what the industry calls “in-network” medical providers, those who have contracts with the insurer. But it doesn’t include claims for care outside those networks. Patients often shoulder more costs for out-of-network services, ramping up the import of these denials.
In recent years, doctors and patients have complained bitterly that insurers are requiring them to get approval in advance for an increasing array of services, causing delays and, in some instances, harm. The government, however, hasn’t compelled insurers to reveal how many requests for prior authorization they get or what percent they deny.
These and other specifics — particularly about which procedures and treatments insurers reject most — would be necessary to turn the government’s data into a viable tool to help consumers choose health plans, said Eric Ellsworth, the director of health data strategy at Consumers' Checkbook, which designs such tools.
A spokesperson for CMS said that, starting in plan year 2024, the agency will require insurers offering federal marketplace plans to submit a few more numbers, including on out-of-network claims, but there’s no timeline yet for much of what advocates say is necessary.
Another effort, launched by a different set of federal regulators, illustrates the resistance that government officials encounter when they consider demanding more.
The U.S. Department of Labor regulates upwards of 2 million health plans, including many in which employers pay directly for workers’ health care coverage rather than buying it from insurance companies. Roughly two-thirds of American workers with insurance depend on such plans, according to KFF.
In July 2016, an arm of the Labor Department proposed rules requiring these plans to reveal a laundry list of never-before-disclosed information, including how many claims they turned down.
In addition, the agency said it was considering whether to demand the dollar amount of what the denied care cost, as well as a breakdown of the reasons why plans turned down claims or denied behavioral health services.
The disclosures were necessary to “remedy the current failure to collect data about a large sector of the health plan market,” as well as to satisfy mandates in the Affordable Care Act and provide critical information for agency oversight, a Labor Department factsheet said.
Trade groups for employers, including retailers and the construction industry, immediately pushed back.
The U.S. Chamber of Commerce said complying with the proposal would take an amount of work not justified by “the limited gains in transparency and enforcement ability.” The powerful business group made it sound like having to make the disclosures could spark insurance Armageddon: Employers might cut back benefits or “eliminate health and welfare benefits altogether.”
Trade groups for health insurance companies, which often act as administrators for employers that pay directly for workers’ health care, joined with business groups to blast the proposal. The Blue Cross Blue Shield Association called the mandated disclosures “burdensome and expensive.” AHIP questioned whether the Labor Department had the legal authority to collect the data and urged the agency to withdraw the idea “in its entirety.”
The proposal also drew opposition from another, less expected quarter: unions. Under some collective bargaining agreements, unions co-sponsor members’ health plans and would have been on the hook for the new reporting requirements, too. The AFL-CIO argued the requirements created a higher standard of disclosure for plans overseen by the Labor Department. To be fair and avoid confusion, the group said, the Labor Department should put its rules on ice until federal health regulators adopted equivalent ones for plans this proposal didn’t cover.
That left the transparency push without political champions on the left or the right, former Assistant Secretary of Labor Phyllis Borzi, who ran the part of the agency that tried to compel more disclosure, said in a recent interview.
“When you’re up against a united front from the industry, the business community and labor, it’s really hard to make a difference,” she said.
By the time the Labor Department stopped accepting feedback, Donald Trump had been elected president.
One trade association for large employers pointed out that the Affordable Care Act, which partly drove the new rules, was “a law that the incoming Administration and the incoming leadership of the 115th Congress have vowed to repeal, delay, dismantle, and otherwise not enforce.”
The law managed to survive the Trump administration, but the Labor Department’s transparency push didn’t. The agency withdrew its proposal in September 2019.
A Labor Department spokesperson said the Biden administration has no immediate plan to revive it.
Ultimately, it’s the National Association of Insurance Commissioners, a group for the top elected or appointed state insurance regulators, that has assembled the most robust details about insurance denials.
The association’s data encompasses more plans than the federal information, is more consistent and captures more specifics, including numbers of out-of-network denials, information about prior authorizations and denial rates for pharmacy claims. All states except New York and North Dakota participate.
Yet, consumers get almost no access. The commissioners’ association only publishes national aggregate statistics, keeping the rest of its cache secret.
When ProPublica requested the detailed data from each state’s insurance department, none would hand it over. More than 30 states said insurers had submitted the information under the authority commissioners are granted to examine insurers’ conduct. And under their states’ codes, they said, examination materials must be kept confidential.
The commissioners association said state insurance regulators use the information to compare companies, flag outliers and track trends.
Birny Birnbaum, a longtime insurance watchdog who serves on the group’s panel of consumer representatives, said the association’s approach reflects how state insurance regulators have been captured by the insurance industry’s demands for secrecy.
“Many seem to view their roles as protectors of industry information, as opposed to enforcers of public information laws,” Birnbaum said in an email.
Connecticut and Vermont compile their own figures and make them publicly accessible. Connecticut began reporting information on denials first, adding these numbers to its annual insurer report card in 2011.
Vermont demands more details, requiring insurers that cover more than 2,000 Vermonters to publicly release prior authorization and prescription drug information that is similar to what the state insurance commissioners collect. Perhaps most usefully, insurers have to separate claims denied because of administrative problems — many of which will be resubmitted and paid — from denials that have “member impact.” These involve services rejected on medical grounds or because they are contractually excluded.
Mike Fisher, Vermont’s state health care advocate, said there’s little indication consumers or employers are using the state’s information, but he still thinks the prospect of public scrutiny may have affected insurers’ practices. The most recent data shows Vermont plans had denial rates between 7.7% and 10.26%, considerably lower than the average for plans on Healthcare.gov.
“I suspect that’s not a coincidence,” Fisher said. “Shining a light on things helps.”
Despite persistent complaints from insurers that Vermont’s requirements are time-consuming and expensive, no insurers have left the state over it. “Certainly not,” said Sebastian Arduengo, who oversees the reporting for the Vermont Department of Financial Regulation.
In California, once considered the most transparent state, the Department of Managed Health Care in 2011 stopped requiring insurance carriers to specify how many claims they rejected.
A department spokesperson said in an email that the agency follows the requirements in state law, and the law doesn’t require health plans to disclose denials.
The state posts reports that flag some plans for failing to pay claims fairly and on time. Consumers can use those to calculate bare-bones denial rates for some insurers, but for others, you’d have to file a public records request to get the details needed to do the math.
Despite the struggles of the last 15 years, Pollitz hasn’t given up hope that one day there will be enough public information to rank insurers by their denial rates and compare how reliably they provide different services, from behavioral health to emergency care.
“There’s a name and shame function that is possible here,” she said. “It holds some real potential for getting plans to clean up their acts.”
READ MORE  Ernesto Rocha-Cuadra died last week at a hospital in Jena, Louisiana, Immigration and Customs Enforcement said. (photo: Sarah L. Voisin/The Washington Post)
Ernesto Rocha-Cuadra died last week at a hospital in Jena, Louisiana, Immigration and Customs Enforcement said. (photo: Sarah L. Voisin/The Washington Post)
Ernesto Rocha-Cuadra died last week at a hospital in Jena, Louisiana, Immigration and Customs Enforcement said.
Ernesto Rocha-Cuadra, 42, died Friday at a hospital in Jena, Louisiana, Immigration and Customs Enforcement said in a statement this week. The preliminary cause of death “was reported by hospital medical officials to be cardiac arrest,” it said.
An ICE panel recommended that Rocha-Cuadra be released in November, a coalition of immigration advocacy groups said in a statement Thursday. The statement said officials at the detention center declined to release him.
“They kept telling him he was going to be released soon,” Frank Rocha-Cuadra, who is Ernesto’s brother and a U.S. citizen, said in the statement from the Shut Down NOLA ICE Coalition. “He was guaranteed he was coming home. Our message is, we want to know what happened to our Ernesto and we will not stop until we find out.”
The coalition said that according to Rocha-Cuadra’s attorneys, he had been petitioning for his freedom and was scheduled for an immigration hearing July 9.
“Ernesto’s untimely death raises many questions that should be investigated at the highest levels. This immigrant prison must be shut down,” Rose Murray, a senior direct services attorney with the Southeast Immigrant Freedom Initiative at the Southern Poverty Law Center, said in the statement.
The statement said that while the details of Rocha-Cuadra’s death were still unclear, his attorneys say that he never mentioned having heart-related medical issues and that his medical records did not indicate heart-related medical issues, either.
ICE did not immediately respond to request for comment on Rocha-Cuadra’s case and whether he had been recommended for release.
Immigration authorities apprehended Rocha-Cuadra after he crossed the border near Andrade, California, on April 17, 2022, according to ICE. On April 26, 2022, he was transferred to ICE custody as he waited for his immigration case to play out.
“ICE incarcerated Ernesto for over a year during which he suffered extensive time in solitary confinement,” the immigration advocacy groups’ statement said.
Rocha-Cuadra’s immigration counsel, Homero López, the legal director of the group Immigration Services and Legal Advocacy, said, “His tragic death after being caged by ICE for more than a year is a reminder of how useless and unnecessary the immigration detention system truly is.”
The immigration groups said Rocha-Cuadra was the fifth person to have died in ICE custody at the Jena detention center since 2016 and the 11th during the Biden administration.
ICE said in its statement this week that it notified the Department of Homeland Security’s Office of Inspector General, the ICE Office of Professional Responsibility and the Nicaraguan Consulate General in Miami of Rocha-Cuadra’s death.
READ MORE 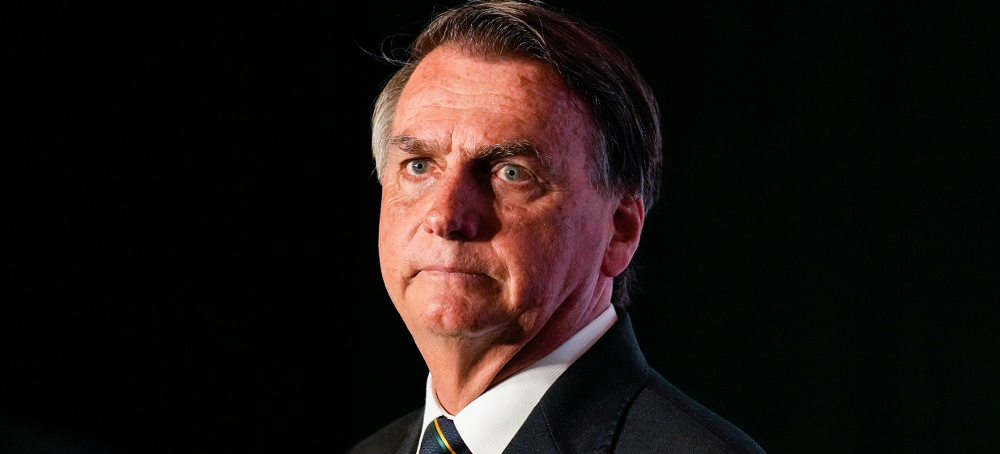 Brazil's Supreme Electoral Court has voted to bar ex-president Jair Bolsonaro from running for office for eight years. (photo: Rebecca Blackwell/AP)
Brazil's Supreme Electoral Court has voted to bar ex-president Jair Bolsonaro from running for office for eight years. (photo: Rebecca Blackwell/AP)
Brazil's Supreme Electoral Court has voted 5-2 to bar ex-president Jair Bolsonaro from running for office for eight years.
He had been accused of undermining Brazilian democracy by falsely claiming that the electronic ballots used were vulnerable to hacking and fraud.
Mr Bolsonaro's lawyers are expected to appeal against the verdict.
They have argued that his statements had no bearing on the election result.
The ban is backdated to 2 October 2022, when the presidential election took place.
If the verdict is allowed to stand, Mr Bolsonaro will not be eligible to take part in the next presidential election in 2026, but will be able to run again in 2030.
He will also be barred from municipal elections due in 2024 and 2028.
Mr Bolsonaro called the decision a "stab in the back" and said he would keep working to advance right-wing politics in Brazil.
The case against the ex-president revolved around a speech he gave while he was still president in 2022.
On 18 July, he invited foreign diplomats to his residence in the capital, Brasilia, where he falsely claimed that the electronic voting machines used in Brazil were prone to being hacked and open to large-scale fraud.
Mr Bolsonaro maintained that he "simply explained how elections work in Brazil" and did not criticise or attack the electoral system.
But the speech came amid a polarising presidential campaign which saw Mr Bolsonaro being challenged for the top job by his arch-rival, left-winger Luiz Inácio Lula da Silva.
The bitterly fought election went into a run-off on 30 October and was won by an extremely narrow margin by Lula.
Mr Bolsonaro never publicly acknowledged his defeat and left Brazil for Florida two days before Lula was sworn in as president.
His supporters, who refused to accept the outcome of the election, stormed Brazil's Congress, the presidential palace and the building housing the Supreme Court on 8 January.
READ MORE 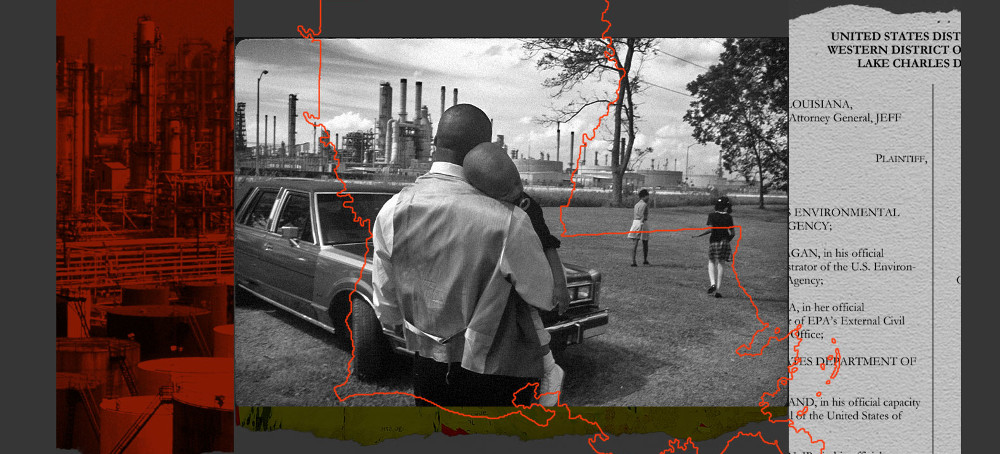 Documents obtained by Grist reveal the sweeping changes that the EPA was negotiating before giving in to GOP pressure. (photo: Andrew Lichtenstein/Corbis)
Documents obtained by Grist reveal the sweeping changes that the EPA was negotiating before giving in to GOP pressure. (photo: Andrew Lichtenstein/Corbis)
Documents obtained by Grist reveal the sweeping changes that the EPA was negotiating before giving in to GOP pressure.
The case hinged on the EPA’s duty to enforce Title VI, a provision of the landmark Civil Rights Act of 1964. Title VI allows federal agencies to take action against state policies that discriminate by disproportionately harming groups protected by the Act — the discriminatory policy being, in this case, Michigan’s permitting of a plant that would pollute Black neighborhoods. After the EPA lost the suit in 2020, agency officials finally began timely investigations of civil rights complaints and made some of the EPA’s first-ever findings of discrimination.
That progress, however, could be short-lived.
This week, the EPA abruptly terminated three of its highest-profile open civil rights complaints. The move deals a major blow not only to the majority-Black communities that filed them but also to the EPA’s own authority to enforce Title VI in places with some of the nation’s worst air quality. The cases originated in the region widely known as “Cancer Alley,” an 85-mile industrial corridor in southeast Louisiana, and were voluntarily closed after the state’s Republican attorney general sued the federal government for alleged abuses of power during the complaint negotiations.
Grist obtained copies of two draft agreements from the now-defunct negotiations, which reveal efforts by EPA officials to institute profound changes to Louisiana’s permitting process, which has historically concentrated chemical plants near Black communities. One of the most substantial terms of the resolution would have required state regulators to assess whether a community is already exposed to disproportionately high levels of pollution before permitting new plants there. With the cases closed, the prospect of those changes has all but vanished.
“This is basically the EPA not using the full power of its environmental laws,” said Adam Kron, a senior attorney at Earthjustice who worked on the case. He described Title VI as one of the clearest ways to advance environmental justice, a goal that Biden EPA has repeatedly called a priority. “It’s disappointing to see EPA acquiesce to what seems like a lawsuit that really doesn’t have much grounding to it.”
The Title VI statute states that no person should, on the basis of race, color, or national origin, be subject to discrimination under any program that receives federal funding. The provision is wide-reaching, covering hundreds of thousands of programs across the country and governing decisions as diverse as where a road can go or who can get treatment at a hospital. But in the environmental space, it’s been largely underutilized, with the EPA routinely failing to respond to dozens of cases within the 180-day period required by the law.
The 2020 federal court ruling on Schmitter’s case gave communities in Louisiana’s St. James and St. John the Baptist parishes hope that Title VI could finally help limit pollution in their backyards. Together, their complaints alleged a number of negligent actions by state regulators, including a failure to curb cancer-causing emissions that violate federal safety standards and to consider pre-existing pollution when permitting new industrial plants. A formal resolution of their cases would have likely addressed these concerns.
The draft agreements that Grist obtained include sweeping measures to change the way the state of Louisiana approves new industrial facilities, like folding community involvement into critical moments of the decision-making process and requiring officials to prove, both before and after plants begin operating, that their emissions will not disproportionately harm people of color. In Louisiana, majority-Black communities are exposed to at least 7 times the emissions, on average, as predominantly White communities in industrial areas.
“We were hoping to get systemic change,” said Kimberly Terrell, a research scientist at the Tulane Environmental Law Clinic, who worked on the complaints. “For decades, people have been fighting against individual polluters and individual facilities, but when the decision-making process itself is flawed, you need something that seeks to improve it.”
Louisiana officials did not respond to a request for comment.
Despite progress with the agreements, testimony in Louisiana’s legal filings suggests that, at some point during the negotiation process, things between state and federal officials began to sour. Then, in late May, the state’s attorney general, Jeff Landry, sued the EPA.
The case hinged on the EPA’s ability to pursue actions based on “disparate impacts,” or the idea that a policy or agency decision can disproportionately harm a specific group of people, regardless of whether or not that harm is intentional. These standards have always been unpopular with some state officials who view them as evidence of federal agencies meddling in matters beyond their authority. The Supreme Court’s conservative majority is sympathetic to these concerns, ruling in numerous landmark cases over the past few years to vastly restrict the powers of federal regulators.
But multiple lawyers that Grist interviewed argued that Louisiana’s legal arguments would have ultimately been unlikely to undermine Title VI, raising the question of why the EPA appears to have preemptively conceded on the matter.
“It was unripe — there was no action by the EPA that Louisiana could challenge,” said Kron. “So it seems like a strange lawsuit for [the federal government] to take as a serious enough threat to just undo this whole process that’s been going on for over a year.”
Environmental advocates and residents in Louisiana also decried the decision to close the complaints.
“I often feel like our communities are left to fight on our own,” said Joy Banner, an activist and long-time resident of the region. “It’s disappointing when we have organizations at the federal level who aren’t willing to step in to fight along with us for our basic human right to survive.”
EPA spokesperson Khanya Brann told Grist that the agency remains “fully committed” to improving the environmental conditions in the communities that filed the complaints.
“Community participation has been critical to identifying both problems and solutions, and we look forward to our continued partnership with the residents in both parishes as we continue our joint efforts to improve public health and the environment,” she said.
The EPA wrote in its letters announcing the closure of the complaints that it would address residents’ concerns through other means, like its pending litigation against one of the region’s most infamous chemical plants and its proposed rules for tightening standards for certain types of facilities operating in the region. But residents told Grist that those measures do not cover the totality of their concerns, and that a major benefit of the Title VI process is its speedy timeline: While court cases can drag on and emissions standards can take years to implement, a resolution of the complaints may have granted communities much faster relief from toxic emissions.
Claire Glenn, a criminal defense attorney with a background in civil rights law, compared EPA’s use of Title VI to other federal agencies’ more robust implementation of the law. The Department of Transportation, for example, requires regulators to consider whether a project will disproportionately impact a group of people before it’s ever constructed. However, she added, deciding where a transit line goes is often less controversial than approving a multi-billion dollar company’s new industrial complex.
“I think the reason EPA’s Title VI program is so hamstrung is because it is so directly butting up against corporate interests,” she said.
Advocates told Grist that they are exploring other options to advance residents’ concerns, and called the EPA’s actions this week a setback but not a roadblock. Residents said that they are determined not to give up.
“We come from a long line of people who fought,” said Banner. “This is just one little hill that we have to overcome — but ultimately I see us heading to the mountain, and victory is the mountain.”
Follow us on facebook and twitter!
PO Box 2043 / Citrus Heights, CA 95611



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.